Imaging does not always help us in treatment of our patient’s pain.
One question that we often hear from prospective new patients is “Do you take X-rays?”
We do not routinely order X-rays, and, in fact, we don’t even have an X-ray machine. If after an examination an X-ray, MRI, or CT (imaging) is deemed clinically necessary, we will order these tests from an outside imaging center.
Most patients are relieved to learn we don’t default to taking X-rays, as they hope to limit their exposure to radiation as well as their costs. Our clinic’s policy on imaging is based on several key pieces of research.
Click on the statements below to learn more about each subject and why we choose to be very conservative with our use of imaging.
According to the American College of Physicians, clinicians should not routinely order X-rays or MRIs for most cases of low back pain.
“Clinicians should not routinely obtain imaging or other diagnostic tests in patients with nonspecific low back pain. ” (1).
The American College of Radiology echoes this finding. In its Appropriateness Criteria, last reviewed in 2015, it states that for a patient with Low Back Pain (2), a general X-ray or MRI of the lumbar spine is usually not appropriate. They conclude that imaging, on the whole, is not warranted in the diagnosis or treatment for these cases.
“It is now clear that uncomplicated acute LBP and/or radiculopathy is a benign, self-limited condition that does not warrant any imaging studies.” (3).
The Journal of the American Medical Association states that “early imaging may precipitate interventions that do not improve outcomes.” Xrays or MRIs early on in treatment may lead to higher costs, more tests and care that do not ultimately help the patient’s condition (4).
Another reason we hesitate before sending patients for X-rays is to avoid unnecessary exposure to radiation, which can pose harmful cumulative effects over time. A 2010 national initiative from the FDA seeks to “reduce unnecessary radiation exposure from medical imaging.” As stated in the initiative,
“In some cases, ordering physicians may lack or be unaware of recommended criteria to guide their decisions about whether or not a particular imaging procedure is medically efficacious. As a result, they may order imaging procedures without sufficient justification and unnecessarily expose patients to radiation (5).”
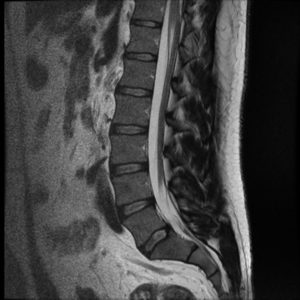
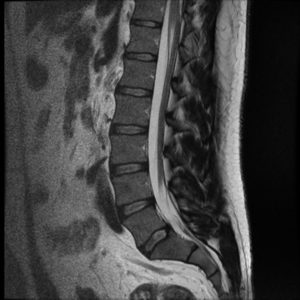
Even advanced imaging such as MRI may not help us and can lead to unnecessary interventions.
Often, there are findings on the radiology reports that tell us about degeneration, tissue damage, or other fear-inducing terms. However, much of these findings may be completely unrelated to your pain, and in fact, even normal.
“Advanced imaging (MRI and CT) are increasingly used in the evaluation of patients with low back pain. Findings such as disk degeneration, facet hypertrophy, and disk protrusion are often interpreted as causes of back pain, triggering both medical and surgical interventions, which are sometimes unsuccessful at alleviating the patient’s symptoms (6).”
Sometimes imaging is unable to tell the difference between old and new damage, which makes it difficult to tell what is actually causing your pain.
Findings on MR imaging within 12 weeks of serious LBP inception are highly unlikely to represent any new structural change. Most new changes (loss of disc signal, facet arthrosis, and end plate signal changes) represent progressive age changes not associated with acute events (7).
And as we age, anatomical changes are a normal part of our lives, and do not always cause us pain.
“Many imaging-based degenerative features are likely part of normal aging and unassociated with pain (8).”
It is often the case that neither an X-ray nor an MRI would even help us in our diagnosis of pain symptoms, as research shows that even imaging can be inaccurate. We also have to be aware of these tests giving us false-positives, or telling us that something is wrong, when it is not. This is true even for imaging of the extremities.
“MRI may be inaccurate in assessing containment status of lumbar disc herniations in 30% of cases (9).”
Inaccuracy can extend to anatomy beyond the spine. As we see in imaging of the knee:
“the true positive rate for complete ACL tear diagnosis with MR imaging was 67%, making the possibility of a false-positive report of “complete ACL tear” inevitable with MR imaging (10).
Capital Chiropractic’s clinical approach is based on current pain management research and patient outcomes. We order X-rays and MRIs only when clinically necessary. If at any time we suspect that it is in the best interest of your health, we won’t hesitate to send you to an imaging center for additional testing.
Learn more about our evidence-based treatments for pain management such as joint manipulation, soft tissue and massage treatments, acupuncture, the McKenzie Method and active rehabilitation exercises, click here.
As always, we are in pursuit of your best life!
To schedule an appointment: Call 515-421-4018 or email office@capitalchirodsm.com.
Citations
- Chou R, Qaseem A, Snow V, Casey D, Cross JT, Shekelle P, et al. Diagnosis and Treatment of Low Back Pain: A Joint Clinical Practice Guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478-491. doi: 10.7326/0003-4819-147-7-200710020-00006
- Defined as: “Acute, subacute, or chronic uncomplicated low back pain or radiculopathy. No red flags. No prior management.”
- Appropriateness Criteria, American College of Radiology.
- Jarvik JG, Gold LS, Comstock BA, Heagerty PJ, Rundell SD, Turner JA, Avins AL, Bauer Z, Bresnahan BW, Friedly JL, James K, Kessler L, Nedeljkovic SS, Nerenz DR, Shi X, Sullivan SD, Chan L, Schwalb JM, Deyo RA. Association of Early Imaging for Back Pain With Clinical Outcomes in Older Adults. JAMA. 2015;313(11):1143-1153. doi:10.1001/jama.2015.1871
- U.S. Food and Drug Administration – Initiative to Reduce Unnecessary Radiation Exposure from Medical Imaging
- Brinjikji, et al., Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol. 2015 Apr;36(4):811-6. doi: 10.3174/ajnr.A417
- Carragee, Eugene et al. Are first-time episodes of serious LBP associated with new MRI findings? The Spine Journal , Volume 6 , Issue 6 , 624 – 635
- Brinjikji, et al., Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol. 2015 Apr;36(4):811-6. doi: 10.3174/ajnr.A417
- Weiner BK, Patel R. The accuracy of MRI in the detection of Lumbar Disc Containment. Journal of Orthopaedic Surgery and Research. 2008;3:46. doi:10.1186/1749-799X-3-46.
- Tsai K-J, Chiang H, Jiang C-C. Magnetic resonance imaging of anterior cruciate ligament rupture. BMC Musculoskeletal Disorders. 2004;5:21. doi:10.1186/1471-2474-5-21.
Image Credits – Radiopaedia:
Normal Lumbar Spine Xray – Case courtesy of Dr Craig Hacking
Normal Lumbar Spine MRI – Case courtesy of A.Prof Frank Gaillard
Normal Cervical Spine Xray – Case courtesy of Dr. Andrew Dixon