So you find out you have a meniscus tear – now what? Is surgery the next step? Could you try physical therapy instead? Are there exercises you can do on your own to make it better? You’ll be surprised by what the research shows below!
What is a meniscus and what are symptoms that it may be torn?
The meniscus is a C-shaped piece of cartilage that acts as a shock absorber between the shinbone (tibia) and the thigh bone (femur). A torn meniscus can result from any activity that causes you to forcefully twist or rotate your knee, such as aggressive pivoting or sudden stops and turns. Even kneeling, deep squatting or lifting something heavy can sometimes lead to a torn meniscus.
Common symptoms of a torn meniscus include but are not limited to:
- Swelling and stiffness
- Pain, especially when twisting or rotating the knee
- Difficulty fully straightening the knee
- “Locked” feeling when moving the knee
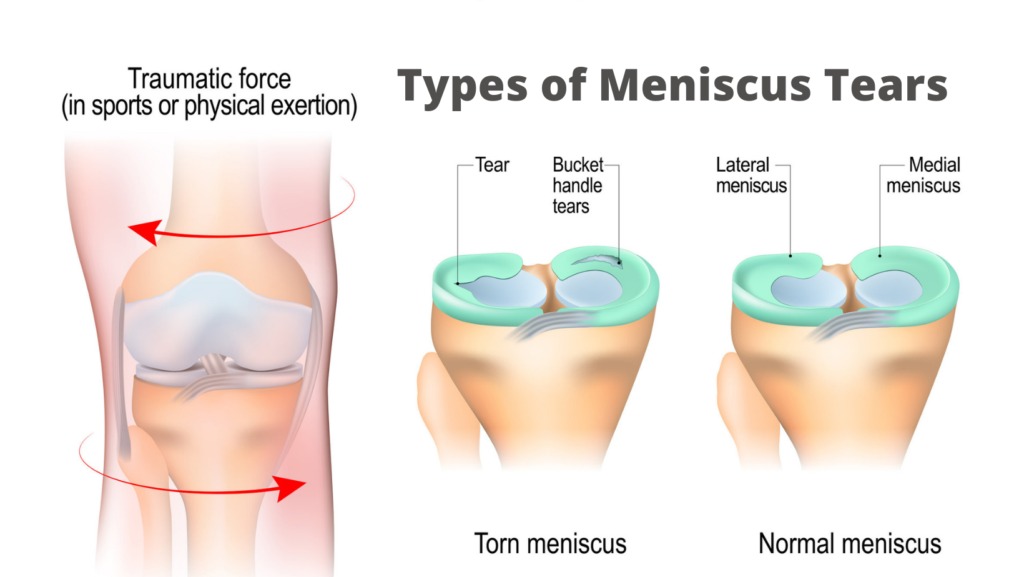
Image from Google images
How can physical therapy help?
A physical therapist can assess and address knee motion, strength, edema (i.e., fluid in the joint), and how you perform functional movements. Education and an individualized exercise program can, in many cases, help to reduce or abolish the symptoms. There are many clinical trials that support using physical therapy as a first option, non-invasive conservative approach, with successful outcomes. (3, 4, 5, 6)
Among patients with nonobstructive (i.e., no locking of the knee joint) meniscal tears, physical therapy was noninferior to Arthroscopic partial meniscectomy (meniscus surgery, or “APM”) for improving patient-reported knee function over a 24-month follow-up period.(1) This tells us that physical therapy may be just as effective as a more invasive surgery.
One research article states that the results of their trial supports current best practice, that physical therapy may be considered an appropriate alternative to surgery, as first-line therapy for patients with meniscal tears.(4, 5) With this study, use of physical therapy is again proven effective and should be considered the standard of care.
And Herrlin et al(6) showed that for middle-aged patients with simple lesions in the meniscus, physical therapy has yielded results as favorable as those of surgery. Because physical therapy is non-invasive, we may begin to think that physical therapy is not only equally as effective, but it should be considered the preferred method over a more invasive surgery.
Meniscus Surgery
You may need surgery if you have a very large tear, or one that causes the knee to lock (pain alone should not be reason for surgery). Surgery could involve one of the following: removal (meniscectomy), repair, or in rare cases, replacement.
Most people tend to have the injured area of the meniscus removed. Arthroscopic partial meniscectomy (APM) is among the most frequently performed procedures in orthopedic surgery. It was estimated that in 2014, over 500,000 meniscectomies were performed in the United States, of which 40% of patients are under 45 years of age. (2,3) This is classified as a minimally invasive surgery.
Despite the minimally invasive nature, studies have shown that patients undergoing arthroscopic meniscectomy have pain, effusion, loss of range of motion (ROM), functional changes, neuromuscular and biomechanical changes, loss of quadriceps muscle strength, and a reduced quality of life (3). If surgery is the best option for you, it’s recommended to have physical therapy after surgery to address the above mentioned issues.
Your meniscus would likely be repaired if the tear was located on the outside region of the meniscus. There’s better blood-flow here, meaning a greater capacity for healing. Repair of the meniscus does require more rehabilitation and may have weight bearing restrictions, use of a locked brace and some restrictions of motion in the first 2-4 weeks. However, a repair of the meniscus does allow better protection and less contact pressure of the knee joint.
Physical Therapy or Surgery?
Whether you have surgery or not, physical therapy is an important component to improving function and your quality of life after a meniscus tear. If you have a meniscus tear, give us a call first! Our physical therapist can answer any questions you may have and work with you to get you back to living your best life. And you may be able to avoid surgery!
References
- JAMA. 2018;320(13):1328-1337. doi:10.1001/jama.2018.13308
- Steiner CA, Karaca Z, Moore BJ, Imshaug MC, Pickens G. Surgeries in hospital-based ambulatory surgery and hospital inpatient settings, 2014. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb223-Ambulatory-Inpatient-Surgeries-2014.pdf. Accessed August 15, 2018.
- Sihvonen R, Paavola M, Malmivaara A, et al; Finnish Degenerative Meniscal Lesion Study (FIDELITY) Group. Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med. 2013;369(26):2515-2524. doi:10.1056/NEJMoa1305189
- Beaufils P, Becker R, Kopf S, et al. Surgical management of degenerative meniscus lesions: the 2016 ESSKA meniscus consensus. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):335-346.
- Stone JA, Salzler MJ, Parker DA, Becker R, Harner CD. Degenerative meniscus tears: assimilation of evidence and consensus statements across three continents: state of the art. Journal of ISAKOS: Joint Disorders & Orthopaedic Sports Medicine. 2017;2(2):108-119.
- Herrlin S, Hållander M, Wange P, Weidenhielm L, Werner S. Arthroscopic or conservative treatment of degenerative medial meniscal tears: a prospective randomised trial. Knee Surg Sports Traumatol Arthrosc. 2007;15:393-401. http:// dx.doi.org/10.1007/s00167-006-0243-2
Share this Post


